Additive manufacturing, or 3D printing, of a kidney model was recently used to help save a patient’s real kidney during a complicated surgery to remove a tumor.
Jay Bishoff, MD, director of Intermountain Medical Center Urological Institute, radiologist Talmage Shill, MD, and collaborators from the Intermountain Healthcare’s Transformation Laboratory in Murray, Utah, converted raw images of CT scans of the patient’s cancerous kidney into a 3D image of the kidney. This digital file was then used to guide the 3D printing of the kidney model.
The team had the model printed in two clear halves so the doctors could examine exactly how the tumor attached to the kidney. The model even allowed the doctors to identify an abnormal “nub” of the tumor that was not evident by just looking at the CT scan. “Without the 3D model, the visual images of the CT scans would not have allowed us to identify this nub prior to the surgery,” said Dr. Bishoff in the press release. “The 3D printing technology allowed us to prepare a more complete plan for the patient’s surgery, show the patient the complexities of the procedure and what would be done during surgery to remove the tumor and save the kidney.”

Cross-section halves of a 3D printed kidney model; Intermountain Medical Center in Murray, UT. (Picture: Al Hartmann | The Salt Lake Tribune)
A different kind of the 3D printed kidney is being used here at Washington University School of Medicine. Sherb Figenshau, MD, Professor of Surgery, Taylor Family and Ralph V. Clayman Chair in Minimally Invasive Urology, is using silicone kidney models derived from 3D printed molds for training surgical residents when performing the robotic-assisted laparoscopic partial nephrectomy. Dr. Figenshau currently has a model of an actual patient’s kidney with an exophytic tumor visible on the surface that will be used in the training.

Silicone kidney with exophytic tumor (bottom) formed using 3D printed mold; one piece of the mold (top); WU
In collaboration with the Washington University Institute of Minimally Invasive Surgery’s (WUIMIS) Biomaterials Lab (Michael Brunt, MD/Jeff Blatnik, MD), Staff Scientist Nick Thompson segmented/rendered the initial kidney model from a patient’s CT scan while Washington University bio-medical engineering student Nabeel Chowdhury transformed the initial kidney model into a 3D printable, hollow, 3-piece mold. Two pieces of the mold form the halves of the kidney; the 3rd piece is a mold of the tumor.

Silicone kidney formed from 3D printed mold, with tumor “excised”; WU
Once the hollow mold was 3D printed, Steven Monda, “a superb biomedical engineering student” according to Dr. Figenshau, filled the mold with silicone to form the actual model of the kidney. The composition of the silicone has been properly adjusted to mimic the color, texture, and consistency of a real kidney. Getting the composition of the silicone just right is based on feedback from surgeons as well as side-by-side testing on pig kidneys to get the “feel” of the silicone as close as possible to that of real kidney tissue. Steven Monda just finished his second year of medical school at St. Louis University, and has started a Master of Science in Clinical Investigation program at WU.
Dr. Figenshau emphasizes that the 3D kidney project has been a team effort. Gerald Andriole, MD, the Robert K Royce Distinguished Chair in Urology and Chief of the Division of Urology, has been a strong supporter of the project and has given guidance in the development of the model. Jonathan Weese, MD, a first year urology resident has worked closely with Nick and Steven developing the model. Barrett Anderson, DO, second year fellow in minimally invasive urology and Baisong Cheng, MD, an international fellow in in urology have worked in applying the model to the robotic simulator in the laboratory.
In the Biomaterials Lab, Nick Thompson works on a multitude of 3D printing projects, including custom fit hernia mesh models that he designed and printed for human abdominal wall models that are anatomically patient-specific. In addition, Nick just finished 3D printing an apparatus that will be used in a specific cell culture experiment here in the Division of Nephrology at WU.
The 3D printing of biological materials, or 3D bioprinting, has recently been made possible because of advances in materials science, cell biology and 3D printing technology. 3D bioprinting has already been used for the generation and transplantation of a variety of tissues such as skin, bone and cartilaginous structures; it is also used for the production of high-throughput 3D tissue models for research, drug discovery and toxicology (see review article in Nature Biotechnology).
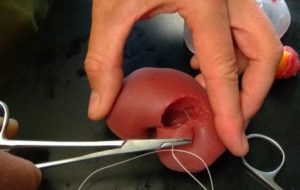
The texture/consistency of the silicone kidney mimics that of real tissue; WU
The WUIMIS Biomaterials Lab has been “getting their feet wet” in the printing of biological materials. The lab has the ability to print cells in predetermined 3D architectures. “We do have two bio-printers in our lab capable of printing living cells, hydrogels, and resorbable plastics,” says Nick Thompson. The lab provides this technology to both the Washington University community and the Greater St. Louis community, as they accept requests for 3D printing service from any interested party (see BioBots’ article on WUIMIS Biomaterials Lab here)
There is no doubt that 3D printing is transforming the face of science, medicine and education. And while the 3D printing of a whole, functioning organ as complicated as the kidney may seem like fantasy, the fast developing technology of 3D printing may just someday make it a reality.